Hammer Toe Signs And Symptoms
 Overview
Overview
Hammer toes (hammertoe) is a deformity of the second, third, or fourth toes. In this condition, the toe is bent at the middle joint, into an upward position, causing it to resemble a hammer (sometimes decribed as ?curled toes?). Left untreated, hammer toes can become inflexible and require surgery. Toes which take on Hammer toe a curled appearance are hammer toes. Mallet toe is a similar condition, but affects the upper joint of a toe.
Causes
The cause of hammertoes varies, but causes include genetics, arthritis and injury to the toe. Treatment for hammertoes depends on the severity and can include anti-inflammatory medication, metatarsal pads, foot exercises and better-fitting shoes. If the pain caused by a hammertoe is so severe that wearing a shoe is uncomfortable, surgery may be necessary. Typically this surgery is an outpatient procedure that doesn?t require general anesthesia, though it is an option. Recovery from surgery usually takes a few weeks, and patients are given special shoes to wear.
 Symptoms
Symptoms
The symptoms of a hammer toe include the following. Pain at the top of the bent toe upon pressure from footwear. Formation of corns on the top of the joint. Redness and swelling at the joint contracture. Restricted or painful motion of the toe joint. Pain in the ball of the foot at the base of the affected toe.
Diagnosis
The treatment options vary with the type and severity of each hammer toe, although identifying the deformity early in its development is important to avoid surgery. Your podiatric physician will examine and X-ray the affected area and recommend a treatment plan specific to your condition.
Non Surgical Treatment
Many people start by treating the problem themselves when they have a painful corn or callus. They try to remove the corn by cutting it off or by applying strong acids, and they try to cushion the toe by applying cushioned pads. Because these treatments can be difficult to perform by oneself (and should never be done by oneself when the patient is diabetic or circulation is poor), and because these treatments only treat the symptom, not the structural deformity that causes their symptom, these treatments can often provide only limited success, and often any success is for only short periods of time. Changes in shoe choices and various types of paddings and other appliances may help, too. For longer-lasting help, we must examine the cause of the deformity. The reason for knowing the cause is that the type of treatment will vary, depending upon the cause of the complaint. Orthotics help control the causes of certain types of contracted toes, (those caused by flexor stabilization, for example), but not other types.
Surgical Treatment
There are several surgical methods to correct a hammer toe. Your physician will decide which method will be most beneficial to you depending on the severity of your deformity, the direction the toe is deviating and the length of the affected toe. Some common surgical methods include. Arthroplasty. To promote straightening, half of the joint located directly underneath the crooked part of the toe is removed. Arthrodesis (fusion) To promote straightening, the joint directly underneath where the toe is crooked is completely removed. A wire or pin is inserted to aid healing. Tendon transfer. Performed alone or in combination with other procedures, a surgeon will take tendons from under the toe and ?re-route? them to the top of the toe to promote straightening. Basal phalangectomy. Performed to assist patients with severe stiffness, this procedure removes the base of the bone underneath the toe. Weil osteotomy. Performed to assist patients with severe stiffness, this procedure involves shortening the metatarsal bone and inserting surgical hardware to aid healing.
Bunion Exercises After Surgery
Overview
 A bunion is the enlargement of the joint at the base of the big toe. It occurs as a result of the misalignment of the bones of the big toe. This leads to stretching of the ligaments and tendons around the big toe joint and causes soft tissue over the joint to become inflamed and painful. There may be additional bone formation (exostosis) in the joint and the skin around the joint may become red and tender. Over time the cartilage in the joint can break down, leading to arthritis.
A bunion is the enlargement of the joint at the base of the big toe. It occurs as a result of the misalignment of the bones of the big toe. This leads to stretching of the ligaments and tendons around the big toe joint and causes soft tissue over the joint to become inflamed and painful. There may be additional bone formation (exostosis) in the joint and the skin around the joint may become red and tender. Over time the cartilage in the joint can break down, leading to arthritis.
Causes
There is much debate as to which is the major cause, but it is likely that your genetic makeup makes you more prone to a bunion or bunionette and that then wearing ill-fitting footwear causes them to develop. Studies have shown that in cultures where people don?t wear shoes but are habitually barefoot, there are very few cases of foot bunions indicating a strong correlation with shoe wear. They are more common in females, most likely due to choice of footwear.
Symptoms
The most obvious symptoms of a bunion are. Pain in the area of the MTP joint, the joint where your big toe connects to your foot. Bending of the big toe in towards the other toes. An enlarged bump of bone or tissue at the MTP joint. Each symptom can range in degree from small to severe. Sometimes the pain can be sufficient to make it difficult to walk in normal shoes. Other symptoms may include. Swelling and inflammation of the skin around the MTP joint. Thickening of the skin in the area of the joint. Restricted motion in your big toe. Pressure from the inward bending of your big toe can affect your other toes, leading to corns on your smaller toes. Ingrown toenails on the smaller toes. Development of hammertoes in the other toes. Calluses on the bottom of your foot. If you have any of these symptoms, especially pain, displacement of your big toe or development of a bulge, you should consider consulting your physician. Even if you're not significantly bothered by some of these symptoms, bunions tend to continue getting bigger and more serious over time and should be taken care of before they do so.
Diagnosis
Bunions are readily apparent, you can see the prominence at the base of the big toe or side of the foot. However, to fully evaluate your condition, the Podiatrist may arrange for x-rays to be taken to determine the degree of the deformity and assess the changes that have occurred. Because bunions are progressive, they don't go away, and will usually get worse over time. But not all cases are alike, some bunions progress more rapidly than others. There is no clear-cut way to predict how fast a bunion will get worse. The severity of the bunion and the symptoms you have will help determine what treatment is recommended for you.
Non Surgical Treatment
Padding with a number of different materials (eg felt) to reduce pressure on the painful prominence of the bunion. Physical therapy can be used to help with the symptoms and improve the range of motion (this is particularly helpful if the pain is coming from inside the joint, rather than from shoe pressure). Manipulation of the joint can be used to help with this (manipulation will never correct the alignment of the joint). Any corns and calluses that are causing symptoms should be treated. The correct fitting of footwear is essential for anyone who is serious about doing something about their bunions and hallux valgus. It may be possible to have your shoes stretched over the area of the bunion to also relieve pressure. Foot orthotics may be useful in helping with the instability about the joint. They may be more helpful if there are other symptoms in the foot as well, as their use in "treating" bunions is controversial. They may play a role in slowing progression and in the prevention of bunions developing again after surgical correction. Exercises can be important in maintaining the mobility of the joint in those with bunions, this is especially important for the arthritic type pains that may be originating from inside the joint and for the prevention of these painful symptoms in the future. 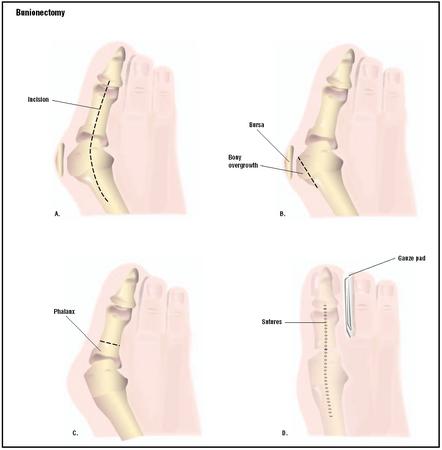
Surgical Treatment
Surgery may be considered if your symptoms are severe and don't respond to non-surgical treatments. The type of surgery will depend on the level of deformity, the severity of your symptoms, your age, and any other associated medical conditions.
Prevention
The best way to reduce your chances of developing a bunion is to wear shoes that fit properly. Any shoe that is too tight or too high will force your toes together and may cause the condition to develop. Shoes need to be wide enough, so they aren't rubbing against the joint, and preferably made of leather. Avoid shoes with a lot elaborate stitching at the front, as this can also cause irritation. Heels should be no more than three to four inches and you should only wear them occasionally. Court shoes should seldomly be worn, as they do not give the foot any support. Be honest with yourself, you know if your shoes aren't fitting you comfortably. Do something about it, or you will suffer for your vanity.
The Facts Concerning Overpronation
Simply put, over-pronation is an excessive or poorly timed pronation which is part of the regular stride. Pronation is when the foot rolls inwards and the arch compresses as part of your normal walking motion. Pronation is necessary for shock absorption to transmit forces up and down our legs. When someone over-pronates, the foot rolls inwards to a greater degree and the arch flattens: this causes the knee and hip to come out of alignment and reduces the function of all the bones in the feet.

Causes
In adults, the most common reason for the onset of Over-Pronation is a condition known as Post Tibial Tendonitis. This condition develops from repetitive stress on the main supporting tendon (Posterior Tibial Tendon) of the foot arch. As the body ages, ligaments and muscles can weaken. When this occurs the job of providing the majority of the support required by the foot arch is placed upon this tendon. Unfortunately, this tendon cannot bear the weight of this burden for too long. Eventually it fatigues under the added strain and in doing so the foot arch becomes progressively lower over a period of time.
Symptoms
People with overpronation may suffer from pain in the knees, hips, and low back. Overpronation itself does not necessarily cause any other symptoms but is a contributing factor of many foot conditions such as Plantar Facsiitis, Heel Spur Syndrome, Posterior Tibialis Tendon Rupture or Tendonitis, Hallux Valgus, Bunion Deformities, Metatarsalgia, Hallux Limitus or Hallux Rigidus, Hammer Toes, and Morton?s Neuroma.
Diagnosis
One of the easiest ways to determine if you overpronate is to look at the bottom of your shoes. Overpronation causes disproportionate wear on the inner side of the shoe. Another way to tell if you might overpronate is to have someone look at the back of your legs and feet, while you are standing. The Achilles tendon runs from the calf muscle to the heel bone, and is visible at the back of the ankle. Normally it runs in a straight line down to the heel. An indication of overpronation is if the tendon is angled to the outside of the foot, and the bone on the inner ankle appears to be more prominent than the outer anklebone. There might also be a bulge visible on the inside of the foot when standing normally. A third home diagnostic test is called the ?wet test?. Wet your foot and stand on a surface that will show an imprint, such as construction paper, or a sidewalk. You overpronate if the imprint shows a complete impression of your foot (as opposed to there being a space where your arch did not touch the ground).

Non Surgical Treatment
Side Step with Opposite Reach. This exercise is designed to load the "bungee cord system" of the gluteal muscle and its opposite, latissimus dorsi muscle to keep the foot from overpronating. Because the opposite arm swings across the front leg when walking, this exercise creates tension in the muscles all the way from the front foot, across the back of the hips and back, to the fingers of the opposite hand. Movement Directions. Stand with left foot on top of the dome of the BT. (Note: For added balance, the right foot can tap on the ground, if needed). Reach right leg out to the side of the BT, and tap the ground while squatting down on the left side and reaching right arm across the left knee. Push down with left big toe while squatting. This activates the arch of the left foot and strengthens all the stabilizing muscles on the left side of the lower body. Return to starting position. Perform 8 to 10 repetitions on each leg.
Prevention
Exercises to strengthen and stretch supporting muscles will help to keep the bones in proper alignment. Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise. Calf stretch: Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times. Golf ball: While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds. Big toe push:
Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions. Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times. Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board.
Does Calcaneal Apophysitis Always Have To Have Surgery Treatment?
Sever disease refers to a calcaneal apophysitis (an inflammation of the apophysis of the heel) which occurs in children and young adolescents. It typically presents in active young children (especially ones who engage in jumping and running sports).
Causes
During the growth spurt of early puberty, the heel bone (also called the calcaneus) sometimes grows faster than the leg muscles and tendons. This can cause the muscles and tendons to become very tight and overstretched, making the heel less flexible and putting pressure on the growth plate. The Achilles tendon (also called the heel cord) is the strongest tendon that attaches to the growth plate in the heel. Over time, repeated stress (force or pressure) on the already tight Achilles tendon damages the growth plate, causing the swelling, tenderness, and pain of Sever's disease. Such stress commonly results from physical activities and sports that involve running and jumping, especially those that take place on hard surfaces, such as track, basketball, soccer, and gymnastics.
Symptoms
Sharp pain will be present in the affected heel (or both heels), especially while running or walking. Pain can be heightened following activity. The area will be tender to the touch and usually becomes inflamed or reddened. It may also be painful to press on the heel with a finger from the back or to squeeze the sides together; the latter is particularly common. You might notice stiffness in some of the surrounding muscles, making regular movements more difficult to achieve. This and the pain can manifest physically in abnormal practices like tiptoeing or limping. In some cases a lump can be detected on the back of the heel, though it may be so small as to defy detection.
Diagnosis
A doctor or other health professional such as a physiotherapist can diagnose Sever?s disease by asking the young person to describe their symptoms and by conducting a physical examination. In some instances, an x-ray may be necessary to rule out other causes of heel pain, such as heel fractures. Sever?s disease does not show on an x-ray because the damage is in the cartilage.
Non Surgical Treatment
Traditional treatment involved simply telling children that they can?t play sport for a year. This is not popular for children or parents and abstaining from sport leads to other problems when wanting to return. Treatments focus on improving foot and lower limb function with footwear selection, heel raises, calf stretching, prescription orthoses, run technique training and training modifications. This results in a reduced load through the growth plate and the child can perform more activity before the growth plate becomes inflamed. Rest will always reduce the Sever?s disease symptoms, however this is always the last option.
Exercise
The following exercises are commonly prescribed to patients with Severs disease. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 1 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Calf Stretch with Towel. Begin this exercise with a resistance band around your foot and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free. Once you can perform 20 repetitions consistently without pain, the exercise can be progressed by gradually increasing the resistance of the band provided there is no increase in symptoms. Bridging. Begin this exercise lying on your back in the position demonstrated. Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds then slowly lower your bottom back down. Repeat 10 times provided the exercise is pain free.
What Are The Primary Causes And Signs And Symptoms Of A Ruptured Achilles Tendon?
Overview
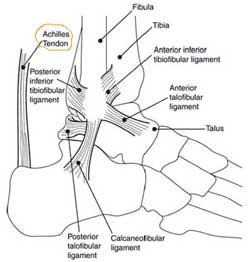 The Achilles tendon is an important part of the leg. It is located just behind and above the heel. It joins the heel bone to the calf muscles. Its function is to help in bending the foot downwards at the ankle (this movement is called plantar flexion by doctors). If the Achilles tendon is torn, this is called an Achilles tendon rupture. The tear may be either partial or complete. In a partial tear, the tendon is partly torn but still joined to the calf muscle. With complete tears, the tendon is completely torn so that the connection between the calf muscles and the ankle bone is lost.
The Achilles tendon is an important part of the leg. It is located just behind and above the heel. It joins the heel bone to the calf muscles. Its function is to help in bending the foot downwards at the ankle (this movement is called plantar flexion by doctors). If the Achilles tendon is torn, this is called an Achilles tendon rupture. The tear may be either partial or complete. In a partial tear, the tendon is partly torn but still joined to the calf muscle. With complete tears, the tendon is completely torn so that the connection between the calf muscles and the ankle bone is lost.
Causes
Repeated stress from a variety of causes is often the cause of Achilles tendon injury. The stress may occur from any of the following. Excessive activity or overuse. Flat feet. Poorly fitting or inadequate shoes. Inadequate warm-up or proper conditioning. Jogging or running on hard surfaces. Older recreational athlete. Previous Achilles tendon injury (tendonitis/rupture). Repeated steroid injections. Sudden changes in intensity of exercise. Use of fluoroquinolone antibiotics (especially in children). Trauma to the ankle. Tense calf muscles prior to exercise. Weak calf muscles.
Symptoms
An Achilles tendon rupture is when the tendon that connects the heel bone to the calf muscle tears and the fibers separate. This happens mostly between the ages of 30 and 50, and usually is caused by sports. Symptoms of Achilles tendon rupture include the following. A pop or snap when the tendon tears. Severe pain in back of the ankle, making it nearly impossible to walk. Swelling and discoloration. Tenderness. Inability to rise on toes. A gap in the back of the ankle where the tendons are separated.
Diagnosis
If an Achilles tendon rupture is suspected, it is important to consult a doctor straight away so that an accurate diagnosis can be made and appropriate treatment recommended. Until a doctor can be consulted it is important to let the foot hang down with the toes pointed to the ground. This prevents the ends of the ruptured tendon pulling any farther apart. The doctor will take a full medical history, including any previous Achilles tendon injuries and what activity was being undertaken at the time the present injury occurred. The doctor will also conduct a physical examination and will check for swelling, tenderness and range of movement in the lower leg and foot. A noticeable gap may be able to be felt in the tendon at the site of the rupture. This is most obvious just after the rupture has occurred and swelling will eventually make this gap difficult to feel. One test commonly used to confirm an Achilles tendon rupture is the Thomson test. For this test the patient lies face down on an examination table. The doctor then squeezes the calf muscles; an action that would normally cause the foot to point like a ballerina (plantar flexion). When a partial rupture has occurred the foot's ability to point may be decreased. When a complete rupture has occurred, the foot may not point at all. Ultrasound scanning of the Achilles tendon may also be recommended in order to assist with the diagnosis.
Non Surgical Treatment
Once the Achilles tendon is partially damaged, one should exercise great care. The risk of rupture is high and if pain is associated with walking, one should consult with an orthopedic surgeon or a sports physician. A complete rupture of the Achilles tendon is never treated at home. It is important to understand that there are no minerals, nutrients, or herbs to treat Achilles tendon injury and any delay just worsens the recovery. 
Surgical Treatment
There are two different types of surgeries; open surgery and percutaneous surgery. During an open surgery an incision is made in the back of the leg and the Achilles tendon is stitched together. In a complete or serious rupture the tendon of plantaris or another vestigial muscle is harvested and wrapped around the Achilles tendon, increasing the strength of the repaired tendon. If the tissue quality is poor, e.g. the injury has been neglected, the surgeon might use a reinforcement mesh (collagen, Artelon or other degradable material). In percutaneous surgery, the surgeon makes several small incisions, rather than one large incision, and sews the tendon back together through the incision(s). Surgery may be delayed for about a week after the rupture to let the swelling go down. For sedentary patients and those who have vasculopathy or risks for poor healing, percutaneous surgical repair may be a better treatment choice than open surgical repair.
Prevention
To reduce your chance of developing Achilles tendon problems, follow the following tips. Stretch and strengthen calf muscles. Stretch your calf to the point at which you feel a noticeable pull but not pain. Don't bounce during a stretch. Calf-strengthening exercises can also help the muscle and tendon absorb more force and prevent injury. Vary your exercises. Alternate high-impact sports, such as running, with low-impact sports, such as walking, biking or swimming. Avoid activities that place excessive stress on your Achilles tendons, such as hill running and jumping activities. Choose running surfaces carefully. Avoid or limit running on hard or slippery surfaces. Dress properly for cold-weather training and wear well-fitting athletic shoes with proper cushioning in the heels. Increase training intensity slowly. Achilles tendon injuries commonly occur after abruptly increasing training intensity. Increase the distance, duration and frequency of your training by no more than 10 percent each week.